
Explainer: how medical oxygen is made
Alongside corticosteroids, medical oxygen is the only proven treatment for Covid-19. As the virus damages a person’s lungs they can experience extremely low oxygen levels in the blood, which can be fatal. Oxygen buys time for the immune system to fight the virus.
A patient hospitalised with Covid-19 may need up to 43 cubic meters of oxygen a day over a two-week stay, an amount that even well-resourced hospitals in the UK and Italy have at times struggled to provide. It is a level of demand that plunged India into such dire straits and has left dozens of other countries on the brink of a similar crisis, as reported by the Bureau this week.
Oxygen is also an essential medicine used to treat pneumonia and sepsis, in anaesthesia and surgery, during childbirth, and to treat trauma victims. But the gap in access to it across different countries is stark: before the pandemic, it is estimated only a fifth of patients in low- and middle- income countries who needed medical oxygen actually received it.
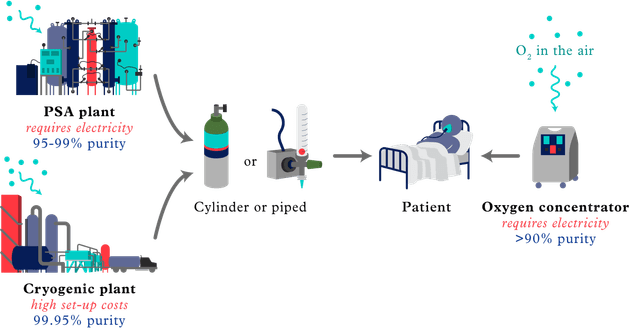
There are three main ways medical oxygen is made.
Cryogenic plants
These are industrial facilities that freeze air so that the oxygen and nitrogen separate and liquid oxygen is formed. Liquid oxygen – which takes up less space than the gas form – is then transported and stored in giant tankers outside hospitals. When it is needed, it is converted back to a gas and piped directly to a patient’s bedside. Cryogenic plants tend to be owned and run by major gas companies, which charge hospitals a fee to deliver the oxygen, fill the tankers and maintain the equipment.
That is how it works in much of Europe and North America. For hospitals in many low- and middle-income countries, however, piped systems are too expensive and poor road infrastructure can affect the delivery of oxygen.
One alternative is to store oxygen as a gas in cylinders, which are kept at the hospital and can be refilled at either a cryogenic plant – where the liquid oxygen can be converted back to gas – or a pressure swing adsorption (PSA) plant. However, these can often be hundreds of miles from a hospital, meaning the cost of transporting cylinders back and forth for refills is huge. Hospitals often have to pay deposit and rental fees for cylinders, and must plan carefully around when they are sent for refills in order to avoid an oxygen shortage on wards. In Nepal, shortages of the cylinders themselves became a problem in April.
All of this means that in many countries oxygen is routinely available only in the big hospitals, leaving patients who live outside of major cities hours away from life-saving treatment.
PSA plants
PSA plants work by taking ambient air and separating the nitrogen from the oxygen, which is left in gas form. In countries such as Uganda and Ethiopia, governments or individual hospitals have invested in PSA plants, which are located very near the hospital and make gas that can be either piped directly to patients or used to refill cylinders.
A PSA plant can vastly improve oxygen access across large areas but for a cash-strapped hospital it is not a cheap solution. They can cost between $100,000 and $1.2m to build, and require trained staff who will need to be paid to work through the night if the plant is to run at full capacity. Their reliance on electricity – another expense – leaves plants vulnerable in areas with erratic power supplies.
Oxygen concentrators
These are portable, suitcase-sized machines that convert ambient air into oxygen. They are often used by hospitals and clinics in rural areas where roads are not good enough to transport cylinders, or in clinics where relatively little oxygen is ever needed.
A concentrator costs between $700 and $3,000, but the amount of electricity it takes to produce a cylinder’s worth of oxygen costs less than $1.50, compared with the estimated $20 – on top of transport and rental fees – that it would cost to source a cylinder of oxygen from a plant.
Concentrators are not a perfect solution. Electricity is not always available and stories of patients dying during blackouts are fairly common. Concentrators are prone to breaking down in hot or humid conditions and many workers describe a “graveyard” of broken machines in hospitals due to an unavailability of either the engineers or parts needed for their repair.
The World Health Organization, Unicef, the World Bank and other donors and NGOs have shipped hundreds of thousands of concentrators to hundreds of countries to help deal with surges in oxygen needs during the pandemic, but companies are now reporting shortages of parts.
Even when oxygen is available, there can be problems identifying the patients with low oxygen levels. In many countries there are shortages of pulse oximeters – small devices clipped to the finger that measure oxygen levels in blood – though this is something the aid agencies are sending along with other equipment.
Reporters: Madlen Davies and Rosa Furneaux
Desk editor: Chrissie Giles
Global editor: James Ball
Investigations editor: Meirion Jones
Production editor: Frankie Goodway
Graphic: Kate Baldwin for TBIJ
This article is part of our Global Health project, which has a number of funders including the Bill and Melinda Gates Foundation. None of our funders have any influence over the Bureau’s editorial decisions or output.
Header image: An oxygen factory in Tocancipá, Colombia.
Credit: Anadolu Agency/Getty
-
Area:
-
Subject:




